Primary brain tumors are cancers that originate in the brain. These tumors are very different from secondary brain tumors, which originally develop elsewhere in the body and spread, or metastasize, to the brain. Primary brain tumors develop from glial cells that support the function of the nerve cells, which are responsible for thought, sensation, muscle control, and coordination. “Glioma” is the name of a tumor that develops from a glial cell.
Gliomas are extremely heterogeneous, including both malignant and non-malignant compartments, requiring analysis of individual cells (as opposed to an average of all cells) to understand glioma biology.
Tumor Infiltrating Lymphocytes (TIL) has been used to effectively treat patients with lung cancer and melanoma. Reproducing similar results in gliomas has been challenging because the brain does not contain a high number of T cells, which are the main immune cells responsible for recognizing and killing cancer. Cancer, including brain tumors, hide from these T cells in order to grow. The few T cells that are able to infiltrate close to and interact with the tumor soon become inert, inactive, and exhausted. Thus, brain tumors do not contain many TILs, and even when T cells are found in brain tumors, they tend to be ineffective. Therefore, here at Duke we have successfully developed a unique new method to isolate TILs using tumor
samples obtained from brain tumor patients.
Our team has recently developed new methods to grow Tumor Infiltrating Lymphocytes (TIL) in the laboratory, making them more active, numerous, and able to recognize the cancer.
The cancer cells have specific proteins (antigens) that are foreign to the individual patient and are recognized as such by the T cell receptors (TCR) so that the T cells and other components of the immune system like antibodies eliminate the cancer cells. Deciphering which TCR recognizes the foreign proteins (antigens) and how they can more efficiently eliminate cancer cells is a very active area of research and holds the key to finding cures for many cancers, including gliomas.
We are working to generate TILs in an efficient, cost-effective manner, to create a protocol that can be transferred to the Duke cell manufacturing facility, and to generate the data the US Food and Drug Administration (FDA) will require before we can conduct a clinical trial in patients. We are also working in parallel on another line of research to improve function and specificity of the TIL to make them more effective before giving them back to patients with glioma to kill the cancer cells more effectively.
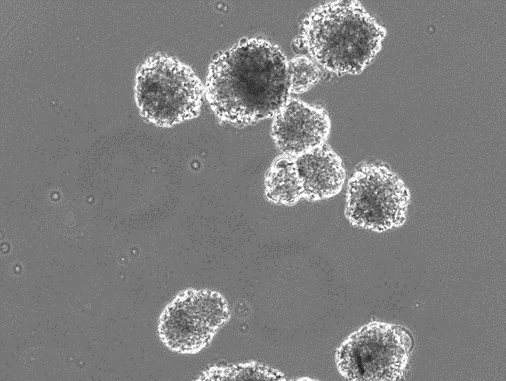
An image of neurospheres – clusters of cells grown in laboratory that mimics the structure and environment of neural tissue
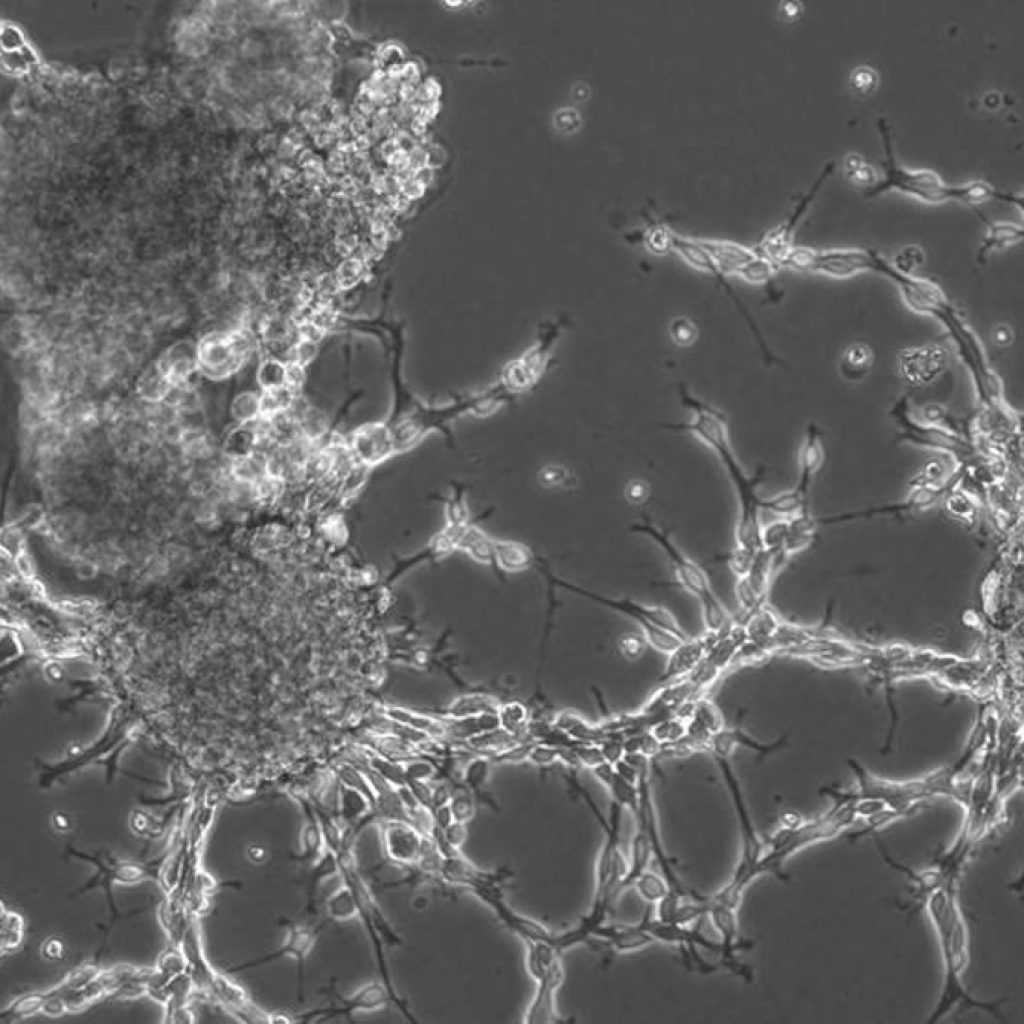
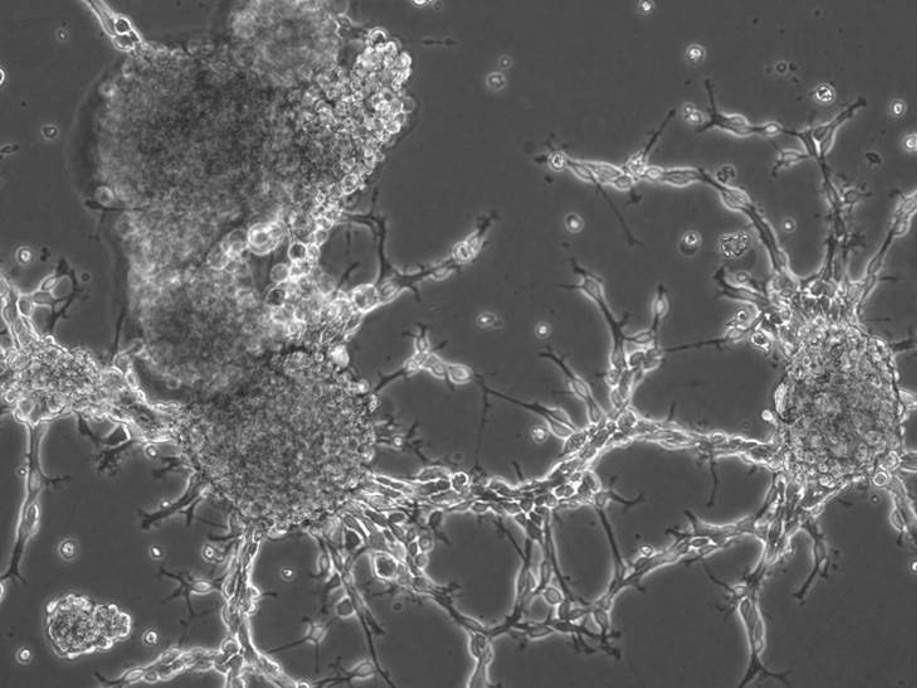
A microscopic view of glioma cells obtained from our patients at the time of surgery and grown in the lab.

Dr. Mustafa Khasraw giving a keynote address at the 2023 European Association of Neurooncology.
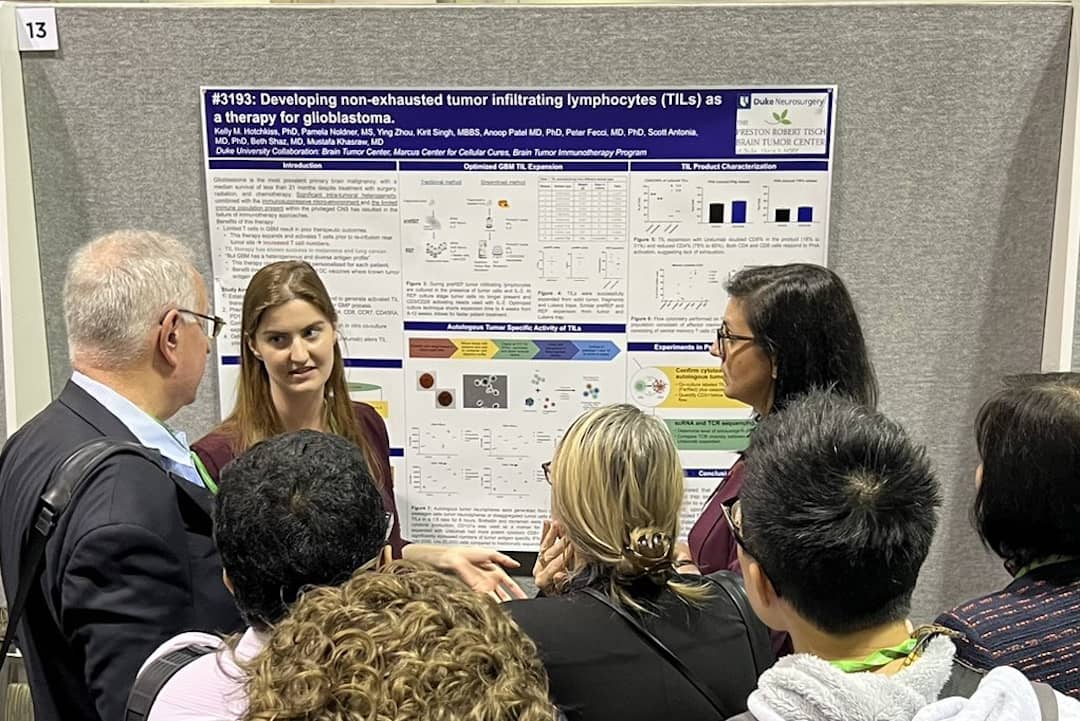
Dr. Kelly Hotchkiss drawing a crowd at her poster presentation on our TIL research at the 2023 American Association of Cancer Research conference.